'Injecting' from the inside (Day 136)

10th October 2014
Most of our prescription medicines are administered orally or by injection. As a patient, the general preference is to receive medicine orally in pill or 'syrup' format. Indeed a phobia or fear of needles is common and with billions of injections given each year that's a lot of nervous patients.
Injections pose other challenges too for patients and medical professionals. There is always a risk of infection caused by piercing the skin, especially from contaminated needles, and medical professionals need to be wary of 'stick' injuries.
But sometimes injections are unavoidable. Drugs made from large proteins can be broken down in the stomach before they can take effect. But what if there was a way to use the powerful acids in our stomachs to deliver an injection in the form of a pill - from the inside?
It seems implausible, but that's what researchers at Massachusetts Institute of Technology (MIT) and Massachusetts General Hospital have managed to do.
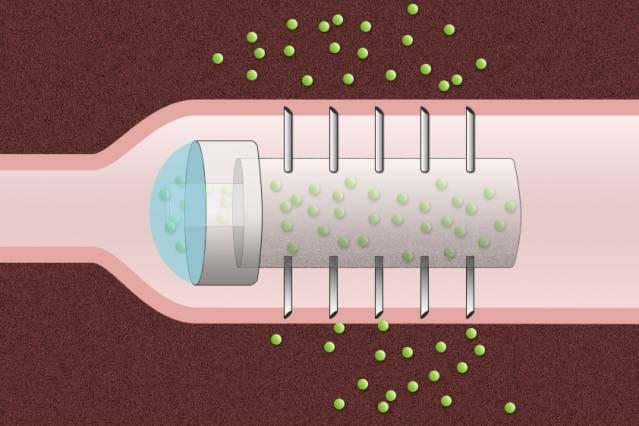
The researchers have devised a novel drug capsule coated with tiny needles that can inject drugs directly into the lining of the stomach after the capsule is swallowed.
The team in Massachusetts believe the development could be a way to circumvent the need to have an infusion or subcutaneous administration of a drug and be very useful for delivering biopharmaceuticals such as antibodies, which are used to treat cancer and autoimmune disorders like arthritis and Crohn’s disease.
This class of drugs, known as 'biologics', also attracted my attention a few days ago in a blog called The Zebrafish Solution.
Schoellhammer and his colleagues set out to design a capsule that would serve as a platform for the delivery of a wide range of therapeutics, prevent degradation of the drugs, and inject the payload directly into the lining of the GI tract.
Their prototype acrylic capsule, two centimeters long and one centimeter in diameter, includes a reservoir for the drug and is coated with hollow, stainless steel needles about five millimeters long.
In animal studies, using pigs, the team found that the capsule delivered insulin more efficiently than injection under the skin, and there were no harmful side effects as the capsule passed through the digestive system.
One of the research team is Carl Schoellhammer, a graduate student in chemical engineering. He said: “The large size of these biologic drugs makes them non-absorbable. And before they even would be absorbed, they’re degraded in your GI tract by acids and enzymes that just eat up the molecules and make them inactive.”
Previous studies of accidental ingestion of sharp objects in human patients have suggested that it could be safe to swallow a capsule coated with short needles. Because there are no pain receptors in the GI tract, patients would not feel any pain from the drug injection.
The tests on pigs showed that it took more than a week for the capsules to move through the entire digestive tract, and the researchers found no traces of tissue damage, supporting the potential safety of this novel approach.
They also found that the microneedles successfully injected insulin into the lining of the stomach, small intestine, and colon, causing the animals’ blood glucose levels to drop. This reduction in blood glucose was faster and larger than the drop seen when the same amount of insulin was given by subcutaneous injection.
The team's plans for the future include modifying the capsules so that peristalsis, or contractions of the digestive tract, would slowly squeeze the drug out of the capsule as it travels through the tract.
They are also working on capsules with needles made of degradable polymers and sugar that would break off and become embedded in the gut lining, where they would slowly disintegrate and release the drug. We wish them good luck.